MedsAware: Deprescribing Action Week

MedsAware is SHPA’s Deprescribing Action Week, 18-24 March 2024, raising awareness around polypharmacy and deprescribing.
On this page:
- Media release: MedsAware 2024 targets inappropriate use of psychotropics in aged and disability care
- A message from...
- Campaign resources
- About poypharmacy, deprescribing and psychotropic medicines
- Our supporters
- Resources and publications
This year, MedsAware will focus on the theme:
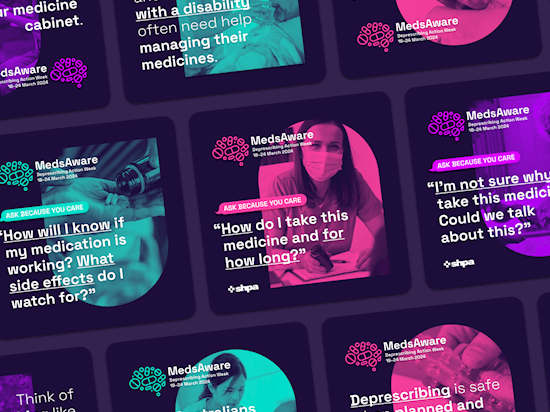
'Ask because you care.'
Medicines can have important benefits in curing and preventing diseases and improving symptoms. However, the potential benefits and harms of medicines can change over time as a person ages, acquires new medical conditions, takes new medicines and changes their care goals. Therefore, medicines should be regularly reviewed to make sure that they are still of benefit, and not causing any harms.
‘Polypharmacy’ refers to the use of multiple medicines, usually defined as the use of five or more regular medicines.
‘Deprescribing’ describes the process of discontinuing medicines that are no longer required, or for which the risk of harm outweighs the benefits in the individual.
Medicines should never be stopped without talking to a doctor or pharmacist.
-
MedsAware 2024, Deprescribing Action Week is about driving conversations around discontinuing medicines that are no longer required, or for which the risk of harm outweighs the benefits.
-
MedsAware seeks to raise awareness around ‘polypharmacy’ and ‘deprescribing’, empowering Australians and their care teams to manage every medicines regimen ensuring it is current, effective and safe.
-
This year’s theme is about empowering older Australians, Australians living with a disability, and their carers, to ask health professionals: “Could any of these medicines be doing more harm than good?” Ask because you care.
#MedsAware supports and raises awareness of Australia’s 10th National Health Priority Area, Quality Use of Medicines and Medicines Safety.
 |
Some questions to ask about your medicinesWhat medications do I need to keep taking, and why? Have any medications been added, stopped or changed, and why? How will I know if my medication is working and what side effects do I watch for? How will this medicine help me? How do I take this medicine and for how long? What are the risks of taking this medicine? What else can I do? I don’t like taking this medicine. I’m worried it’s giving me side effects, or I don’t think it is working. Could you please review it? I’m not sure why I take this medicine. Could we talk about this? I would like you to please review if I still need this medicine. Could I possibly stop taking this medicine? |
Sources:
https://www.choosingwisely.org.au/assets/NPSMW2464_GMBH_5-QuestionsAboutYourMedicines.pdf
https://www.ismp-canada.org/download/MedRec/5questions/MedSafetyPoster-CaDeN-EN.pdf
https://onlinelibrary.wiley.com/doi/10.1111/bcpt.13938
A message from...
tr>
Dr Mike Freelander MPFor #MedsAware 2024, Mike Freelander MP, Federal Member for Macarthur (NSW) and Chair of the Standing Committee on Health, Aged Care and Sport, discusses the importance of our deprescribing message.
|
Senator the Hon Anne RustonFor #MedsAware 2024, Senator the Hon Anne Ruston (SA), Shadow Minister for Health and Aged Care, encourages us to think about the medicines we're taking.
|
Senator Hollie HughesFor #MedsAware , Senator Hollie Hughes (NSW), Shadow Assistant Minister for Mental Health and Suicide Prevention and Deputy Chair of the Joint Standing Committee on the National Disability Insurance Scheme, speaks on medicines-related harm, psycotropic medicines and the importance of deprescribing.
|
Spread the #MedsAware message!Help spread the message! Here you can find social media images and posters. Make sure to tag SHPA and use the hashtag #MedsAware in your posts. |
|
|
Purple Pen Podcast episode159 - Deprescribing psychotropics with Dr Mark HorowitzThe Purple Pen Podcast - named for the pen colour of choice for hospital pharmacists - is a podcast produced for, but not limited to, pharmacists and health professionals. Their latest episode, Deprescribing psychotropics with Dr Mark Horowitz, has been released to coincide with MedsAware 2024. Join Kristin as she talks with Dr Mark Horowitz about how to deprescribe psychotropics like antidepressants, what is known about the causes of depression, what evidence is behind the antidepressants commonly used, what the symptoms of antidepressant withdrawal look like and the origins of the phrase "it's Bedlam here." The episode will be available on Spoitfy and Apple Podcasts on Sunday 16 March 2024. |
|
|
|
|
|
|
Inappropriate use of psychotropic medicines
|
 |
— SHPA President, Tom Simpson |
 |
ADeN Acting Chair Dr Lisa Kouladjian O’Donnell says as people age, their priorities and life values change, and their medicine regimen should reflect their goals of care.
— ADeN Acting Chair, Dr Lisa Kouladjian O’Donnell |
 |
— FIP CEO, Dr Catherine Duggan |
 |
— AMA President, Professor Steve Robson |
 |
COTA Chief Executive Officer, Patricia Sparrow, says a national focus on deprescribing which centres the needs of patients is important.
— COTA Chief Executive Officer, Patricia Sparrow |
 |
— CATAG Chair, Anita Shutt |
 |
Dr Nicole Higgins, says it is a complex area of medicine that required careful management.
— RACGP President, Dr Nicole Higgins |
Proudly supported by:
 |
 |
 |
 |
 |
|
 |
 |
Australian Deprescribing Network (ADeN) The Australian Deprescribing Network (ADeN) involves clinicians, academic researchers, policy makers, students and consumers working together to develop the evidence-base, clinical guidance and knowledge translation to facilitate deprescribing of medicines that are no longer providing benefit or are causing harm. ADeN aims to promote research, awareness, practice and policy for the safe and appropriate use of medicines for all Australians. Visit their website to:
Follow ADeN on X: @DeprescribeAU |
 |
International Pharmaceutical Federation (FIP) The International Pharmaceutical Federation (FIP) is the global body for pharmacy, pharmaceutical sciences and pharmaceutical education. Through our 156 national organisations, academic institutional members and individual members, we represent over four million pharmacists, pharmaceutical scientists and pharmaceutical educators around the world. Click here for the history of FIP. |
 |
Royal Australian College of General Practitioners (RACGP) The Royal Australian College of General Practitioners (RACGP) is the peak representative organisation for general practice, the backbone of Australia’s health system. We set the standards for general practice, facilitate lifelong learning for GPs, connect the general practice community, and advocate for better health and wellbeing for all Australians. |
 |
Council on the Ageing (COTA) COTA Australia is the leading advocacy organisation for older people. |
 |
Registry of Senior Australians (ROSA) The Registry of Senior Australians (ROSA) is a national multisectoral integrated data platform designed to monitor and evaluate the health, service use, social welfare, medication use, mortality, and other outcomes of >3.5 million people who received or are receiving aged care services nationally. |
 |
Council of Australian Therapeutic Advisory Groups (CATAG) CATAG is a collaborative incorporating all Australian State and Territory Therapeutic or Medicines Advisory Groups. CATAG is an expert and consensus-based collaboration that influences clinical governance so that a quality use of medicines approach is considered in both policy and practice. CATAG is dedicated to optimising medicines use and promoting the safe, effective, equitable and sustainable use of medicines. CATAG facilitates information and knowledge exchange, provides guidance, and advocates for best practices in therapeutic decision-making. |
 |
Australian Medical Association (AMA) The Australian Medical Association (AMA) is the peak professional body for doctors in Australia. The AMA promotes and protects the professional interests of doctors and the healthcare needs of patients and communities. Representing doctors, the AMA works with governments to develop and influence health policy to provide the best outcomes for doctors, their patients, and the community. The AMA represents and supports all Australian doctors and medical students. They are member-run and led, fighting for fairness and equality, and lobby and campaign on the issues affecting the medical profession. |
Resources and publications
Australian Deprescribing Network (ADeN)
The Australian Deprescribing Network (ADeN) comprises of clinicians, academic researchers, policy makers, students and consumers working together to develop the evidence-base, clinical guidance and knowledge translation to facilitate deprescribing of medicines that are no longer providing benefit or are causing harm.
Choosing Wisely Australia (choosingwisely.org.au)
The Choosing Wisely Australia initiative is helping the healthcare community and consumers to start important conversations about unnecessary and sometimes harmful tests, treatments and procedures. We are here to support consumers to make informed decisions in partnership with their healthcare professionals in ways that suit their own preferences and personal circumstances. Choosing Wisely is challenging the notion that ‘more is always better’. The right choice should be based on the best available evidence and discussion between you and your healthcare team.
- Primary Health Tasmania, A guide to deprescribing fact sheet, principles and medicines-specific information.
- NSW Therapeutic Advisory Group Inc., Deprescribing Tools, guides and consumer information, developed by a translational research project team led by Professor Sarah Hilmer.
- Desprescribing.org, Canadian initiative hosting deprescribing guideline resources and related research, co-led by Drs Lisa McCarthy, Wade Thompson and Barbara Farrell.
- AMH Online: Aged Care Companion, deprescribing guide
- Reeve, Emily. "Deprescribing tools: a review of the types of tools available to aid deprescribing in clinical practice." Journal of pharmacy practice and research 50.1 (2020): 98-107.
- Evidence-Based Clinical Practice Guideline for Deprescribing Opioid Analgesics (University of Sydney) ->
- Evidence-based Clinical Practice Guideline for Deprescribing Cholinesterase Inhibitors and Memantine (University of Sydney)
- RACGP aged care clinical guide (Silver Book) Part A: Deprescribing
- Medicines reconciliation. A toolkit for pharmacists (2021)
- Patient safety: Pharmacists’ role in “Medication without harm” (2020)
- FIP Statement of policy on the role of pharmacists in patient safety (2020)
- Use of medicines by the elderly: The role of pharmacy in promoting adherence (2018)
- Medicines Stewardship (CATAG), which inclides Guiding Principles for Medicines Stewardship Programs, the Medicines Stewardship Toolkit, Medicines Stewardship Program Flowchart, and their Medicines Stewardship webinar.
- Psychotropic Medicines in Cognitive Disability or Impairment Clinical Care Standard | Australian Commission On Safety And Quality In Health Care
Key publications
- Liacos, M., et. al. Deprescribing in older people, Aust Prescr 2020;43:114-20. DOI ->
- Manski-Nankervis J., et. al, Prescribing and deprescribing in chronic kidney disease, AJGP Vol. 50, No. 4, April 2021.
- Quek, H.W., et. al, Deprescribing considerations for older people in general practice, AJGP, Vol. 52, No. 4, April 2023.
- Scott IA. Deprescribing: a 20-year retrospective. J Pharm Pract Res 2023, 53: 320-327. https://doi.org/10.1002/jppr.1906
- Thompson W, Reeve E, McDonald EG, Farrell B, Scott S, Steinman MA, Morin L, Lundby C. Ten deprescribing articles you should know about: A guide for newcomers to the field. Basic Clin Pharmacol Toxicol. 2023 Dec;133(6):661-664. doi: 10.1111/bcpt.13877. Epub 2023 May 4. PMID: 37142559; PMCID: PMC10831497.
- Vasilevskis E.E., et. al., Deprescribing medications among older adults from end of hospitalization through postacute care: A Shed-MEDS randomized clinical trial. JAMA Intern Med 2023; 183: 223–31. Summarised in ‘Time to “shed some meds” among older people at hospital discharge and post-acute care’, Samantha Fraser, SHPA MedsScan Geriatric Medicine, Issue 2, 2023.
- Woodward, M.C., Deprescribing: Achieving Better Health Outcomes for Older People through Reducing Medications, J Pharm Pract Res 2003; 33: 323–8. DOI ->
Clinical Resources
- Deprescribing considerations for older people in general practice, AJGP, https://www1.racgp.org.au/ajgp/2023/april/deprescribing-considerations-for-older-people-in-g
- Deprescribing proton pump inhibitors, AJGP, https://www1.racgp.org.au/ajgp/2022/november/deprescribing-proton-pump-inhibitors
- Standards for general practice residential aged care
- https://www.racgp.org.au/running-a-practice/practice-standards/standards-for-other-health-care-settings/standards-for-gp-residential-aged-care
- Hilmer SN, Gnjidic D. The anticholinergic burden: from research to practice. Australian prescriber 2022;45(4):118–20.
- Hilmer SN, Gnjidic D. Prescribing for frail older people. Australian Prescriber 2017;40:174-78. doi: 10.18773/austprescr.2017.055
- Hilmer S, Gnjidic D. Statins in older adults. Aust Prescr 2013;36(3):79-82.
- The anticholinergic burden: from research to practice. Aust Prescr https://australianprescriber.tg.org.au/articles/the-anticholinergic-burden-from-research-to-practice.html
- Limiting antipsychotic drugs in dementia Aust Presc https://australianprescriber.tg.org.au/articles/limiting-antipsychotic-drugs-in-dementia.html
- https://deprescribing.org/case-reports/ - several case reports on different deprescribing case studies
References:
1. https://www.psa.org.au/advocacy/working-for-our-profession/medicine-safety/take-care/
2. https://www.agedcarequality.gov.au/resource-library/psychotropic-medications-used-australia-information-aged-care#:~:text=What%20are%20psychotropic%20medications%3F&text=The%20three%20main%20classes%20of,classes%20include%20anticonvulsants%20and%20stimulants.
3. Song, M.; Ware, R.; Doan, T. N.; Harley, D. (2019). Psychotropic medication use in adults with intellectual disability in Queensland, Australia, from 1999 to 2015: a cohort study. Journal of Intellectual Disability Research, (), jir.12685–. doi:10.1111/jir.12685
4. Song M, Ware RS, Doan TN, et al. Appropriateness of psychotropic medication use in a cohort of adolescents with intellectual disability in Queensland, Australia. BJPsych Open 2020;6(6):e142. At: www.ncbi.nlm.nih.gov/pmc/articles/ PMC7745239/pdf/S2056472420001258a.pdf
5. Exhibit 3-61, Sydney Hearing, Statement of Juanita Westbury, 29 April 2019, WIT.0117.0001.0001 at 0008 [13]; J Westbury et al. ‘More action needed: Psychotropic prescribing in Australian RACFs’, Australian and New Zealand Journal of Psychiatry, 2019, Vol 53, 2, p 139 (Exhibit 3-2, Sydney Hearing, general tender bundle, tab 49, RCD.9999.0032.0128).
6. Tran HTM, Roman C, Yip G, Dooley M, Salahudeen MS, Mitra B. Influence of Potentially Inappropriate Medication Use on Older Australians' Admission to Emergency Department Short Stay. Geriatrics (Basel). 2024 Jan 4;9(1):6. doi: 10.3390/geriatrics9010006. PMID: 38247981; PMCID: PMC10801464.